Did you know that up to 40% to 50% of couples with difficulty conceiving have a degree of male factor? In fact, male infertility is just as common as female infertility.
Believe it or not, sperm production is a delicate and complicated process that requires several organs to work in tandem. That’s why, when couples are struggling to get pregnant, it’s important to assess the fertility of both partners.
There are many tests to determine the cause of male infertility, one of which is a semen analysis. So, what is a semen analysis report and what information can it determine about a man’s sperm count and/or his level of unhealthy sperm?
Here we will explain the sperm analysis process and the results you can expect from a sperm test.
What Is Semen Analysis?
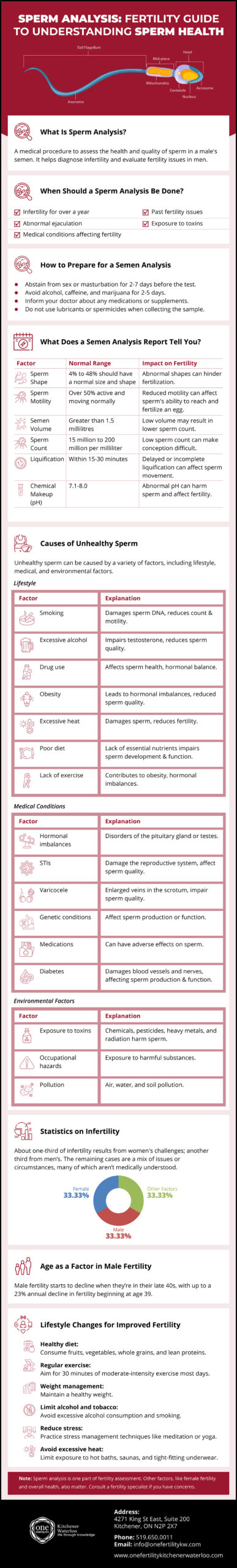
Semen analysis, also known as a sperm count test, measures the levels of healthy and unhealthy sperm a man has, as well as the sperm’s viability. This test will analyze the semen—the fluid containing sperm that is released during ejaculation.
When Should a Sperm Analysis Be Done?
If you and your partner have been unsuccessful in your attempts to get pregnant for over a year, you may want to get a sperm analysis done. A semen analysis will determine if low sperm count or sperm dysfunction could be the reason behind the infertility.
Having a low sperm count or having unhealthy/low-quality sperm can decrease your chances of getting your partner pregnant.
You may also want to get a sperm analysis if you have a history of any of the following issues:
- Erection or ejaculation problems
- Low sex drive
- Pain, discomfort, a lump, or swelling in the testicle area
- A history of testicle, prostate, or sexual issues
- A groin, testicle, penis, or scrotum surgery
- Vasectomy reversal
Alternately, sperm tests can also be conducted after a man has undergone a vasectomy. Your doctor may recommend getting a sperm analysis once a month for three months to determine if there is anymore sperm present in the semen.
How Is Semen Analysis Performed?
In order to test the male partner’s semen, your doctor will require a semen sample.
Typically, this involves ejaculating into a sterile cup in a private room at the doctor’s office via masturbation. The male partner also has the option of collecting his sample at home; however, you need to ensure the sample is kept at body temperature and that it is brought to the lab within an hour of collection. In this case, the doctor may provide you/your male partner with a special condom or a sterile cup to collect the semen sample.
Precautions to Take before Semen Analysis
To ensure the semen sample is viable, your doctor may require the male partner to abstain from sex or masturbation for a minimum of two days and a maximum of seven days before the sperm test.
The male partner should also avoid alcohol, caffeine, and marijuana for approximately two to five days before the sperm analysis. If the male partner’s taking any prescription medications or herbal supplements, make sure to inform the doctor before providing a sperm sample.
When collecting the sperm sample, do not use any lubrications or spermicides.
What Are the Causes of Unhealthy Sperm?
There are many reasons for unhealthy sperm, such as:
- Lifestyle
- Smoking
- Obesity
- Stress
- Depression
- Above-average alcohol consumption
- Drug use
- A previous STI
- Sperm abnormalities
- Ejaculation problems
- Vasectomy
- Prolonged heat exposure
- Chemical exposure
- Hormone imbalances
- Certain medications
It is also possible to get an abnormal semen analysis report due to contamination of the sample. It may be recommended to repeat the test to confirm results are out of normal range.
What Does a Semen Analysis Report Tell You?
Once the doctor has the sperm sample, the lab technician will look at it under a microscope. By conducting a semen analysis, the lab tech and doctor can determine the following seven factors:
1. Sperm Shape
The shape and size of the sperm can affect a man’s fertility. Typically, 50% of the sperm needs to be normally shaped or it could reduce fertility. When conducting a sperm test, the lab will look for abnormalities in the sperm’s head, middle, or tail. Sometimes, sperm could be immature and unable to fertilize an egg.
2. Movement
Next, the lab tech will look to see how many sperm are moving and how they are moving. Ideally, 50% of the sperm should be active and moving normally for an hour after ejaculation. The sperm will be rated on a scale of 0 to 4 based on its movement, with 0 meaning the sperm are not moving and 4 meaning the sperm have good movement.
3. Volume
The lab will also make note of how much semen the male patient was able to provide in the sample. Normally, patients should be able to provide at least 1.5 millilitres or half a teaspoon. A low volume of semen could result in a lower sperm count to fertilize an egg; meanwhile, a high volume of semen could mean the sperm present are diluted.
4. Sperm Count
Typically, the normal sperm count for a semen analysis is between 15 million and 200 million per millilitre of semen. This is also known as sperm density. If the sperm count is too low, it will make it harder to conceive, as fewer sperm are present to fertilize the egg.
5. Liquification
Normally, semen is thick during ejaculation, but it should liquify within 15 to 30 minutes. It’s important for semen to liquify in order to move sperm. If semen doesn’t liquefy or it takes too long for liquification to occur, there may be a problem with the male’s fertility.
6. Chemical Makeup
A lab tech will examine the chemical makeup, particularly the pH levels, of the semen during a semen analysis report. A normal pH is between 7.1 and 8.0. Anything lower indicates that the male patient has acidic semen, or his ejaculatory ducts are blocked; meanwhile, anything higher means the man’s semen is alkaline and he may have an infection. An abnormal pH could result in unhealthy sperm.
7. Viability
The analysis will include obtaining data on the percentage of live sperm in your sample. This differentiates between live non motile sperm and dead sperm. The assessment of pre-incubation motility and post-incubation motility will provide an understanding of the viability of ejaculated sperm. Sperm should survive in the women’s reproductive track for several days.
Semen Analysis at ONE Fertility Kitchener Waterloo
At ONE Fertility Kitchener Waterloo, we provide our patients with the best comprehensive fertility care and guidance. Whether you require a semen analysis or are looking for ways to improve your chances of conceiving, our team of compassionate, experienced, and open-minded nurses, physicians, technicians, and administrative staff are with you every step of the way.
To learn more about our fertility clinic, our treatment options for unhealthy sperm, or to discuss your semen analysis report, give us a call or send us an email and we would be happy to answer any questions you might have.





